I got the call on Thursday about 3:35. I had just lain down for a nap about 10 minutes before, but I was instantly and totally happily awake.
Mom had a ‘spidey sense’ of urgency the last week of June, and ended up coming down on Wednesday, so she was already down from Asheville with us. They gave me until 4:30 or 5 to get to the hospital and check in admitting, so it was just enough time for Kevin to get away from work in Greensboro and run in for a minute.
It felt really odd to check in Admitting- everything was super quiet in the area. It also felt very awkward to take a ride upstairs in a wheelchair when I could still walk. After this ride, the awkwardness went away. I guess the change into the hospital gown for the suite of labwork and chest x-ray assessments made it all feel official. There was a sense of urgency to get to the hospital and have assessments done, but they didn’t yet know when the donor OR time would be- and then what my OR time would be. They were guessing around 9pm and midnight. I was cautioned many times prior to this day and on this day that the plug could be pulled on the transplant even up to me being on the operating room table if anything was not as it should be. I was expectant and ready, but it all felt surreal. I wasn’t going to allow myself to believe everything was set in stone until I was on the table.
The biggest thing that struck me as we were waiting was that every nurse and medical provider kept asking, “Is this your first time?” We were a little bewildered at first, but soon realized that they kept asking because many people are called in as a secondary person on the list and have to go through all the assessment in case the primary doesn’t work out- and many people have to come in multiple times before the liver quality is right or they are healthy enough for surgery. The medical staff was so excited that it was my first call and that things seemed to be a go [as were we!].
The waiting wasn’t so bad. It seemed to fly by for me. My in-laws were able to get to the hospital fairly quickly, Kevin & Mom came with me, and my Dad and Sister were able to get here in plenty of time before surgery. I got a call from my District Superintendent and from Bishop Hope Morgan Ward! Dad’s new DS happened to be close by and dropped in to pray with me as well. My church member who works in the Children’s hospital was working that night, and able to come say hello and offer hospitality to my family. In all of these things, it did not feel too long. Nine o’clock came and passed, and 10:00, and then we finally got word that my OR time would be 12:30. [For all those who wondered about ceasing to eat or drink before surgery- that was no problem after all (~4pm-12:30am). Maybe some calls happen more quickly, but they know how to deal with it.]

A nice fellow from Kenya with the same first name as my mom’s dad came to wheel me down to the Pre-OP area, where they did the last bit of checking and preparation and I got my blue hat signaling I was ready for surgery. It was incredibly quiet. There was only one other patient in this massive area, writhing with pain that they were waiting to be controlled before they took him to surgery. It was nice to be surrounded by my family. I felt like I definitely had the best position, though. I got to be unconscious and get a new liver- they had the hard job of waiting in the middle of the night in chairs designed for people not to fall asleep in. Someone was very nice and brought them all heated blankets and self-fluffing pillows to arrange themselves for the wait.
The surgeons were very happy. They came out to check with the family a few times. The major concern was that the donor liver would be too large, but they reported it was the perfect size. The blood and bile connections started working immediately with no leakage. They *almost* didn’t put a drain in, but did anyway. It did not drain much, and I only had it a few days. They only gave me blood because my hemoglobin was a little low, not because of blood loss. The surgery was projected to last between 6-8 hours [up to 12 by some estimates], but my surgery only took 4 hours. I was breathing on my own before I left the OR! Grace upon grace.
I stayed in the ICU for 36 hours. I really don’t remember it except in little snippets. I remember my nurse’s face, my sister and husband cooling my face and hands and feet with washcloths as requested, glimpsing Angel and Catherine. Maybe I would remember more if prompted, but that is ok. I apparently moved to a chair facing the window for a while, which made my family really happy. I took a walk soon afterward, and have a vague memory of that. I do not remember having an ultrasound [which I think Kevin and Dad had never seen one of before, so they were super-fascinated by the color overlay and sound of fluids moving through vessels], but I do have a tactile memory of having a panel pushed behind my back for an Xray.

My hospital stay to me consisted of my room on the transplant floor, which is just fine! Thankfully, I looked up some lists people had posted online of hospital ‘go’ bags. I was so glad I bought a pillow to go behind the small of my back and under my legs, knowing I would have to sleep on my back the entire time [I’m a side sleeper!]. The one night in the hospital in March killed my back, so I knew I needed something. My back still hurt by the time I went home, but not nearly as badly. I also got some socks with grippers on the bottom, and some chemical dry shampoo. If someone is going to be in the hospital for a while- these things are all great. I wish I had packed a nice fleece blanket and my own pillow. When I could eat regular food, I was grateful for my husband running to get me my favorite foods from out. I was itchy a lot in the hospital due to a reaction with IV pain medicine and several adhesives, so the pillowcases were super scratchy to me sometimes. I solved that by laying a t-shirt over my pillow at night for something softer.
They took me off my IV after a few days. I was a little itchy, likely due to the IV pain medicine. Liver numbers are expected to be extremely high after transplant, and then drop every day with the anti-rejection medicines. My numbers dropped initially, but rose again after a few days in the regular room. Due to this, I had a CT scan about 1:30 am one morning and had to have a liver biopsy (most liver transplant patients have to have at least 1). They wanted me to have access to IV pain medicine during this and a longer doppler study. Unfortunately, they put me back on the same IV pain medicine, which made me increasingly itchy. I spent one night unable to keep from clawing my skin. I had a cool washcloth, thankfully, that I used to calm my skin. It would heat up and then feel cool again after a few minutes. I did get some Benadryl. After the biopsy results came back, it showed I had moderate rejection of the liver. The doctors solved this by giving me three huge doses of steriods. The dose they gave me at nighttime made me wide awake. I slept pretty well every other night in the hospital. After the first night or two in my normal room, I was only woken up at midnight and 6 am for medicine and labwork. I really hated the lancets they used in the hospital to test blood sugar. That is one of the best things about being home- no more blood sugar testing prior to each meal. My fingertips are grateful.
I am so grateful for the medical team that worked with me. The liver PA that checked me into the hospital and guided us through the first day was with us all the way ’til discharge (except for one day off). He was spunky, awesome, caring-and you would think he had known me personally for years beforehand. All the nurses I had went above and beyond basic requirements of my care and for their job (except 1- but I’m certain there must have been something(s) going on on the floor that took her attention). I loved talking with them and appreciated their concern for me. For instance, I asked one nurse for a hot pack early on. From that point on, she brought me more unasked whenever she came into the room. How awesome! When we saw her on walks in the hallway (when she wasn’t my nurse for the day) she would get super excited at my progress and exclaim how much better I looked! Another nurse turned out to also be a Pastor’s Kid, have lived in Greensboro, and many other commonalities. It was sweet that she took time to have nice conversations with us [I think this came at expense of her lunchtime and dismissal time a lot!].
I’m grateful too for the outpouring of love from those who know me and those who don’t. Whether it was prayer, sharing beads for the awesome representation of my journey, cards, creating or contributing to our you caring site, or many other ways, I am grateful. No major life event goes without wrinkles- and mine have been small ones- but they’re much easier to iron out with the support of a community. For church folks and others that can’t wait to see me, I am working on a means for you to do so. Just remember I am an introvert! This doesn’t mean I don’t want to see you. Being an introvert means you feel all the stimuli in your environment to a greater extent than extroverts. It takes a lot more to process and deal with all of it, and it can be overwhelming. Hence, quiet time is necessary. I have quite a lot of stimuli in my environment with my healing incision and medication, etc. I want to and will see you (as long as you are not sick or might be getting something contagious)! Details to come. We are still also trying to get the blood levels of my main anti-rejection drug to the right level (and consistently).
In the hospital, I couldn’t bear to watch or read the full extent of news stories of more unnecessary, UNDESERVED, horrific deaths of black men, nor of the unacceptable, tragic deaths of police in Dallas. Persons of color and police officers matter- not more, not less- and it breaks my heart when other persons treat these groups as if their lives are worthless, expendable, and not created in the image of our same Creator.
Earlier in the day, Facebook popped up a memory of a status I had shared from a devotional. I broke down in tears trying to read it out to my family, of God’s love and perseverance. The passage linked to it was from Ezekiel 36:25-26 (MSG).
I’ll give you a new heart, put a new spirit in you. I’ll remove the stone heart from your body and replace it with a heart that’s God-willed, not self-willed.
The text isn’t talking about a literal organ, of course. But, I had just had an angry, red, knotty (looking like it was going to turn to stone) liver removed, and a new beautiful purple healthy liver put in as the greatest gift of my life. [You can see pictures-if you want- at the bottom of my Recovery Photos page.] I broke down in thankfulness, thanksgiving and awe. But I also broke down in pain for the loss of lives that occurred that week in the long line of lives that have already been wrenched away unnecessarily. I thought about our hearts’ fleshiness as a nation. Those who have felt as I felt have hearts of flesh. The ‘problem’ with new, fleshy organs is that they are delicate. You have to take care of yourself and them. Each new event is felt and has an impact. But having an organ of stone is a major problem that only leads on the road to death.
I was awake the night of July 7, having had my trip home delayed so that I could receive 2nd and 3rd doses of IV steroid. As I was awake, I prayed and lamented for all those in the past week who never dreamed they weren’t going to get to go home. I read psalms of lament and prayed for my friends of color- especially who are raising children with gorgeous brown skin tones, for my friends and their loved ones in law enforcement, and for the hardness of hearts. The warmth and grace of receiving a new liver and gift of life met cold front of pain and lament and made a storm in my soul. This storm will continue to simmer and drive my actions, this Holy Spirit storm in my fleshy heart. I pray that through the praise and lament, my heart may never be replaced by stone.
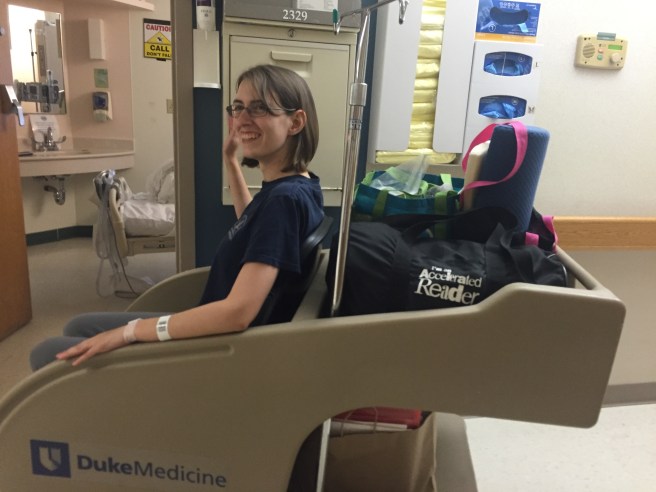
The next day, Friday the 8th, I came home. I know it’s hard, but don’t take your bed and a warm shower for granted. These things are glorious!
Since I’ve been home, I’ve had lots of trips to the doctor for regular labs, lots of naps, snuggles with kitties, great meals, and much more. I’ve been taking walks down the street, trying to exercise as encouraged and avoid the bending, pulling, pushing and lifting as instructed.

I got my staples out on Tuesday, a few days earlier than the usual 21 days! I feel very aware of my incision right now, and I know my job right now is to rest, and to be rather than to do (while doing the things I love that I can). Your job, my friends with fleshy hearts, is the same. Grace be upon you, as it has poured out mightily upon me.

 Just walked in the door at home with my new liver! Gosh, it feels so good to be home.
Just walked in the door at home with my new liver! Gosh, it feels so good to be home.